Obstetrics
Every pregnancy and birth is unique, and we strive to support your vision of the perfect experience with the goal of healthy mom and healthy baby. We support a wide range of delivery options, including: natural childbirth, labor support with our Midwife, Deanna Farmer-CNM, pain control with epidural, C-Section and VBAC. We enjoy caring for both low-risk and high-risk obstetrical patients. Some high-risk conditions we commonly care for include; advanced maternal age, multiples, diabetes, hypertension, IVF and previous cervical or uterine surgery. In the event that our patients have questions or needs after office hours, we have a physician on call 24 hours per day.

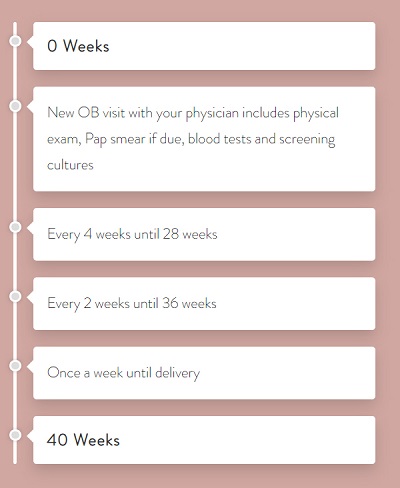
If your pregnancy is complicated, more frequent visits may be necessary. It is advisable to make two or three appointments in advance. Please be assured that we make every effort to run on schedule; however, emergencies do occur. Please make sure we have your current telephone number and email address, as we may need to call, text or email you to inform you that we are running behind. If you cannot make an appointment, please call and cancel at least 24 hours in advance. If you deliver, we will automatically cancel subsequent appointments.
Routine Prenatal Labs – Labs performed on or before your first visit may include blood count, blood type and Rh, Rubella, urinalysis, hepatitis screen, syphilis serology, pap smear, gonorrhea culture, chlamydia culture, HIV testing, urine culture. Hemoglobin Electrophoresis, CMV, HbA1C, thyroid level or toxoplasmosis titer, if necessary.
First trimester bleeding/risk of miscarriage
Thirty percent of women bleed in the first trimester of pregnancy. Women always worry that this indicates a miscarriage, but at least 50% of those who bleed do not miscarry. An ultrasound can help us diagnose if miscarriage is a risk. Call us if you have bleeding so that we can determine if you need a visit or an ultrasound. It is fine to wait to call during normal business hours unless you have one of the following signs, which might require emergency care:
- Bleeding – soaking more than a pad per hour
- Persistent large blood clots
- Severe, intolerable cramping
Genetic Screening (Optional)
If you have certain risk factors, including advanced maternal age or a positive family history, you may have genetic testing that will screen for the most common chromosomal abnormalities seen in pregnancies. This testing can also tell us what the sex of your baby is and can be done after 10 completed weeks of pregnancy.
AFP – Screening for probabilities of some genetic disorders including neural tube defects. This test can be done after 15 weeks.
We also offer an optional gender scan around 16 weeks to determine the sex of your baby. This ultrasound is not typically covered by insurance and therefore a cash payment will be due the time of the appointment.
Ultrasound
Ultrasound uses high frequency sound waves to produce a picture of your baby. This imaging is performed right here in our offices by one of our highly skilled sonographers. An anatomy ultrasound is routinely done around 20 weeks gestation to check the baby’s heart, brain, spine, kidneys, etc. At this visit, the sex can usually be seen if not already known.
Additional ultrasounds are performed based on the medical need, such as elevated blood pressure, diabetes or a fundal height that does not correlate with gestational weeks.
One-hour Glucose test
All patients will get a blood sugar test during their sixth month of pregnancy to screen for gestational diabetes. We recommend fasting for a few hours before this test. You will be provided with the glucose solution when you arrive for your appointment which you will drink in 5 minutes. At the end of your appointment, or when an hour has passed, your labs will be drawn to test your glucose level.
Complete Blood Count
We will also screen your blood to evaluate for possible anemia at the time of your glucose screening. If your levels are below a certain threshold, which is common during pregnancy, you may be started on iron supplements.
Rh Immunoglobulin injection (if Rh negative)
If your blood type is Rh negative, then you may be at risk for a blood type incompatibility. This is a pregnancy complication in which your immune system attacks the baby’s blood cells if you have a negative blood type and your baby has a positive blood type. Fortunately, it can be prevented with a shot called Rhogam which is given at 28 weeks or anytime vaginal bleeding occurs. If you are Rh negative, contact our office immediately.
TDaP Vaccine
TDaP is a vaccine that protects against tetanus, diphtheria and pertussis (whooping cough) in people who are 11-64 years of age. The TDaP vaccine is recommended for all pregnant women in their 3rd trimester regardless of previous vaccinations. This is to protect the baby from transmission of whooping cough in its first few months of life. While not usually a serious illness in adults, whooping cough can be fatal to newborn babies. Other family members and caregivers should be current in their vaccine as well to help protect the baby (it is due every 10 years in non-pregnant adults).
Group B Strep Vaginal Culture
Group B streptococcus (GBS) is a type of bacteria that can be found in a pregnant woman’s vagina or rectum. This bacteria is normally found in about 25 % of all healthy, adult women. Because a mother can pass GBS to her baby during delivery and antibiotics can decrease the risk of infection significantly, any mother who tests positive will require IV antibiotics during labor. GBS is responsible for illness in about 1 in every 2,000 babies in the United States.
When Should You Go to the Hospital
We welcome your questions. If possible, please hold routine questions for your regular prenatal visits. If you have questions that need to be addressed, please call our office during regular office hours. Our nursing staff can answer many of your questions or will find out the necessary information from one of our doctors and will relay the information to you. If your questions require that you speak directly to a physician, please be aware, we generally return calls during the late afternoon when we have finished seeing patients. If you have an emergency, please tell our receptionist the nature of your problem so that it may be handled immediately.
Although you are seen regularly during your pregnancy, you may have some questions and/or problems which occur between your visits to the doctor’s office. Notify your physician or nurse if any of the following conditions outlined below should occur:
- You have any severe pain
- You experience persistent uterine cramping, backaches, or contractions of any frequency prior to 36 weeks (one month before your due date or earlier).
- You do not feel your baby move for several hours after 28 weeks or if you think there is a significant decrease in your baby’s activity (less than 10 movements in 2 hours).
- You are having regular painful contractions every five minutes or less for one hour and are more than 36 weeks.
- You think your water has broken, regardless of presence/absence of contractions. Repetitive leakage or a gush of fluid from the vagina.
- If you have a temperature greater than 101 degrees.
- Abdominal trauma or car accident
Medications Safe During Pregnancy
- COLDS/Cough: Benadryl, Dimetapp, Ocean Nasal Spray, Tylenol Cold, Actifed, Sudafed, Robitussin, Robitussin-AC, Robitussin-DM, Triaminic Syrup, Delsym
- Constipation: Surfak, Dialose Stool Softeners, Metamucil, Colace, Miralax
- Diarrhea: Donnagel, Kaopectate, Imodium, Liquid Imodium
- Hemorrhoids: Annusol, Preparation H
- Indigestion: Maalox, Mylanta, Tums, OTC Pepcid, Zantac 75, Natural Papaya Enzyme Tablets
- Insomnia: Benadryl 25-50mg, Tylenol PM
- Leg Cramps: Calcium Tablets, Increase Dairy Products
- Nausea: Emetrol
- Rash: Benadryl 25mg (1 every 8 hours)
- Sore Throat: Cepacol Lozenges, Extra Strength Tylenol

